Incarcerated Patients in the Emergency Department: Advocating for Our Patients
Incarcerated Patients in the Emergency Department:
Advocating for Our Patients
Wriitten by Diana Halloran, MD
The first time I took care of an incarcerated patient I was a third-year medical student on my internal medicine rotation. This patient was shackled to his bed, and I wondered how I would complete my physical exam. Since then, I have taken care of more incarcerated patients within the emergency department, all shackled to their stretchers. I remember thinking – how do I do a neurological exam? I can’t assess their lower extremity strength; I can’t ask them to walk to assess their gait. And I didn’t know if I could ask the guards to remove the shackles to assist with my exam.
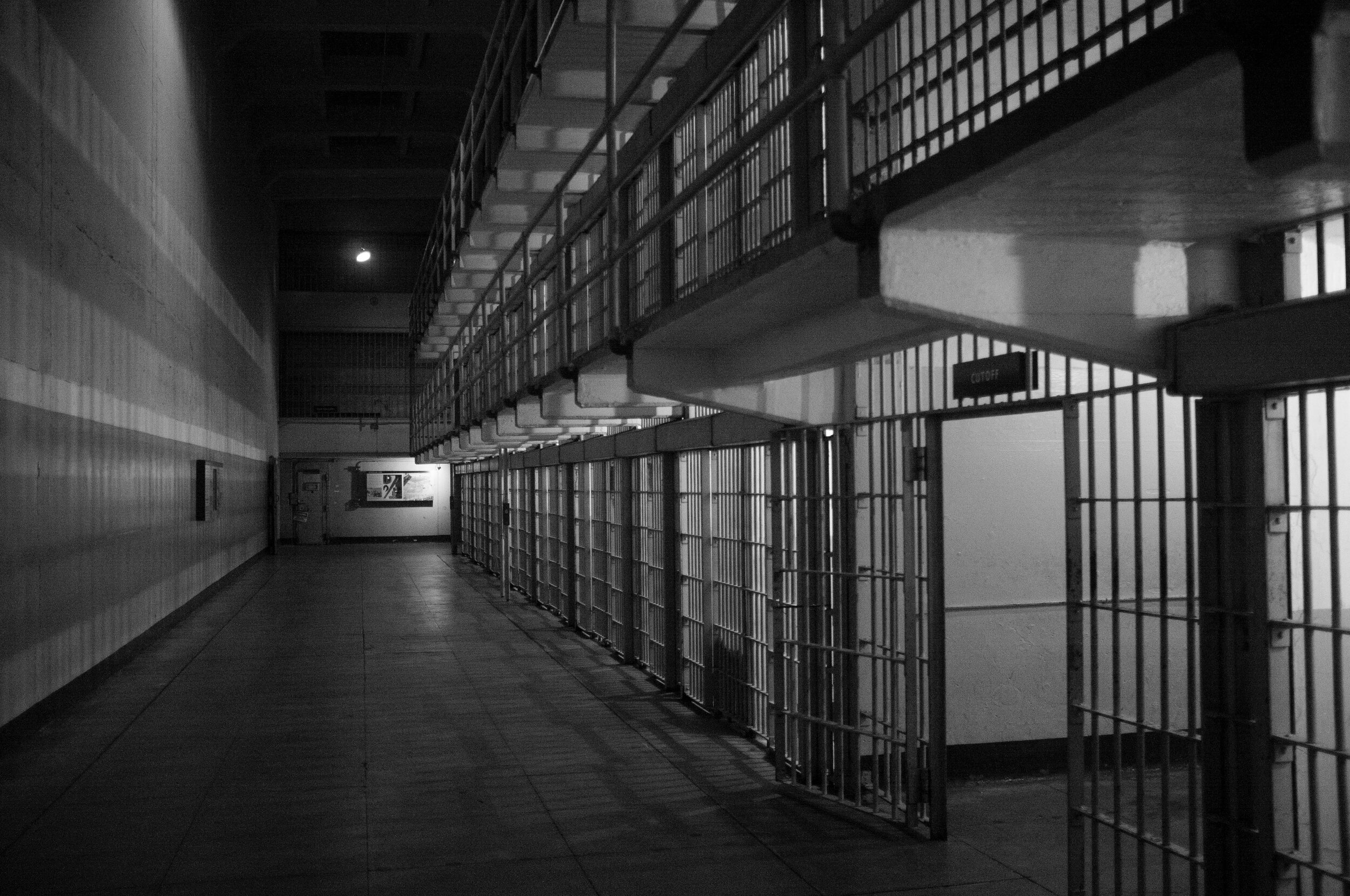
There are more than 2 million incarcerated people in the United States as of 2018. As with the general population, many incarcerated people have chronic health issues or comorbidities that bring them to the emergency department. Correctional medicine is a unique blend of health policy and law, medical practice, and ethics. Learning about healthcare of incarcerated patients is critical for emergency physicians to appropriately advocate and care for our patients.
Right to healthcare
Under the Eight Amendment and the 1976 Supreme Court Case Estelle v. Gamble prison officials are required to provide incarcerated people with healthcare – as withholding medical care amounts to cruel and unusual punishment. Cases following this decision have continued to emphasize three important rights of healthcare: right to access care, right to care ordered by a health professional, and right to professional medical judgment. EMTALA, of course, does apply to incarcerated patients. No matter who a patient is we must provide them with care.
HIPAA
Patient-physician confidentiality and the protection of public health information via the HIPAA privacy rule is a strong and important pillar of the practice of medicine. Of course, there are notable exceptions such as suspicion of child or elder abuse, or when a patient presents with injuries due to a firearm which some states require mandated disclosure.
But for incarcerated patients, how might the patient-physician relationship change? Are incarcerated patients still granted the same right to a private health relationship? The American Hospital Association guidelines say hospitals are not required to disclose private health information without obtaining patient authorization or unless one of the following circumstances are met: subpoenas, warrants, or summonses, if the patient might be the victim of a crime, if the patient is in fact present at the hospital, or if any criminal conduct takes place. The American College of Emergency Physicians states that private health information about an incarcerated patient should not be released unless there is permission from the patient, surrogate decision maker, or a legal requirement. If these situations are met and private health information is provided to law enforcement or correction officers, this should be thoroughly documented in the medical record.
Shackling of Pregnant Incarcerated patients
When it comes to management of pregnant incarcerated women, the American College of Obstetrics and Gynecology emphasizes that the use of restraints may put the health of both the patient and the fetus at risk. The process is demeaning, hardly necessary, and can interfere with medical evaluation. This would ring true as well for the emergency physician. Completing a thorough physical exam is impossible when the patient is shackled to the stretcher. Physicians have the right to advocate for the removal of restraints from pregnant incarcerated patients to better evaluate and serve our patients.
There has been an abundance of policy changes regarding the shackling of incarcerated pregnant women. The Second Chance Act, signed into law in 2008, required federal prisons to report and justify any time pregnant female prisoners were shackled. Then in 2018 the First Step Act prohibited the use of restraints and shackling on incarcerated women from pregnancy through postpartum recovery. However, both of these laws are only applicable to federal prisons, and therefore State and county prisons, where the majority of incarcerated women are, do not have to abide by these laws.
Although there is no federal law regarding shackling of non-pregnant patients, as their physicians we can advocate to remove their handcuffs as well. Many of the same arguments for not shackling pregnant incarcerated patients applies to non-pregnant incarcerated patients: it can affect their medical evaluation, it is demeaning, and it is hardly necessary as incarcerated patients are accompanied by corrections officers or law enforcement. Our arguments might not be granted, but it is our ethical duty to try.
Refusing Healthcare & Unnecessary Testing
The intersection between healthcare and law enforcement is blurry, especially in emergency medicine where physicians might be frequently cross paths with local police. Anecdotally, law enforcement has been known to ask for tests or labs which they do not have the authority to ask for. There have been cases of professional repercussions when not following these requests – such as a nurse who was arrested after she refused to draw blood for a police officer from an unconscious patient. Emergency physicians might face similar outside pressure to obtain unnecessary labs or testing on incarcerated patients– such as a blood alcohol level or urine drug screen. This becomes even more confusing for emergency physicians when law enforcement or correction officers present a warrant asking for labs or imaging to rule out drugs, alcohol, or body packing, that the patient refuses.
There is precedence in Supreme Court law relating to this topic. Rochin v. California in 1952 was a case in which an unwilling patient forcibly had a nasogastric tube placed and was given emetic solution after he was found swallowing unknown capsules. The Supreme Court ruled that the brutality used to determine the contents of the capsules “shocks the conscience” and physical abuse cannot be used to obtain incriminating evidence
Emergency physicians do not have to follow warrants asking for invasive tests or procedures, especially if not clinically indicated or if the patient refuses. Emergency physicians should be aware that incarcerated patients, just as patients in the community, have the right to refuse medical care or procedures assuming they have capacity. However, warrants might be able to compel patients to undergo non-invasive testing such as blood alcohol levels. Our responsibility is with the patient, and we should use our professional medical judgement to determine if the test or procedure is appropriate or indicated. It might be prudent to discuss specific situations preemptively with a hospital risk manager and a medical director.
Proxy Decision Making & Code Status
While incarcerated patients have the same rights as patients in the community regarding their own medical decision making, how might their status as incarcerated change other aspects of their care? What if they are incapacitated? All patients, including incarcerated patients, have the right to designate a surrogate decision maker. Wardens, guards, and law enforcement officers are not court-appointed legal guardians and cannot make medical decisions for incarcerated patients. This claim has legal precedent in the case of Davenport vs the Estate of Marquette F. Cummings in 2014 when an incarcerated patient was brought to the emergency department after he was stabbed in the eye. The warden for the facility included instructions on the patient’s paperwork that he was to be “Do Not Resuscitate”, and the patient was removed from life support. The patients family sued the warden, and the case was brought to the 11th U.S. Circuit Court of Appeals, where the warden was deemed to be lacking the authority to make end of life decisions for prisoners. The warden then asked the Supreme Court to review the case – which they declined.
To facilitate care, emergency physicians should ask incarcerated patients if they have a decision maker in cases of emergency or incapacitation and document this in their medical chart. Physicians and other medical staff owe incarcerated patients the same ethical duty as other patients regarding their appointed surrogate. Code status should follow the same guidelines with the patients reporting their own preference if able to, and their healthcare surrogate reporting if the patient is incapacitated. If the patient has no designated medical decision maker, then the surrogacy ladder system may be used from spouse to children to parents and so on. If no legal medical decision maker can be found, then the court might appoint someone to this role.
Further Action
The intersection of law, policy, and healthcare are evident when discussing incarcerated patients. As emergency medicine physicians, it is important to be familiar with the healthcare inequities and healthcare ethical situations that incarcerated people face. Some other topics to familiarize yourselves with include pain management, hunger strikes, palliative care, reproductive health and sexual violence, psychiatric disorders, and infectious diseases – including COVID-19.
Incarcerated patients often have their healthcare rights violated by healthcare staff, including emergency physicians. These violations can arise from healthcare staff being unfamiliar with the existing laws and policies (just as my own experience in medical school), or from intimidation from law enforcement or corrections officers. Emergency physicians should do their best to familiarize themselves on the rights of incarcerated patients and should contact their hospital risk manager or medical director for guidance if needed. In one survey of 184 physicians, 98.4% or 181 physicians were unaware of existing guidelines for the treatment of prisoners in general hospitals. It is imperative that the care of prisoners including ethics and law be a standard aspect of medical training.
Emergency medicine has been rooted in advocacy since its inception, and advocacy for incarcerated patients is no different. We need more policy and medical organization guidelines regarding the rights of incarcerated patients in order to help guide interactions between patients, emergency physicians and staff, and law enforcement or corrections officers within the emergency department.